Parkinson’s Disease Psychosis (PDP)
Around 50% of patients with Parkinson’s disease may experience hallucinations and/or delusions over the course of their disease.
Around 50% of patients with Parkinson’s disease may experience hallucinations and/or delusions over the course of their disease.
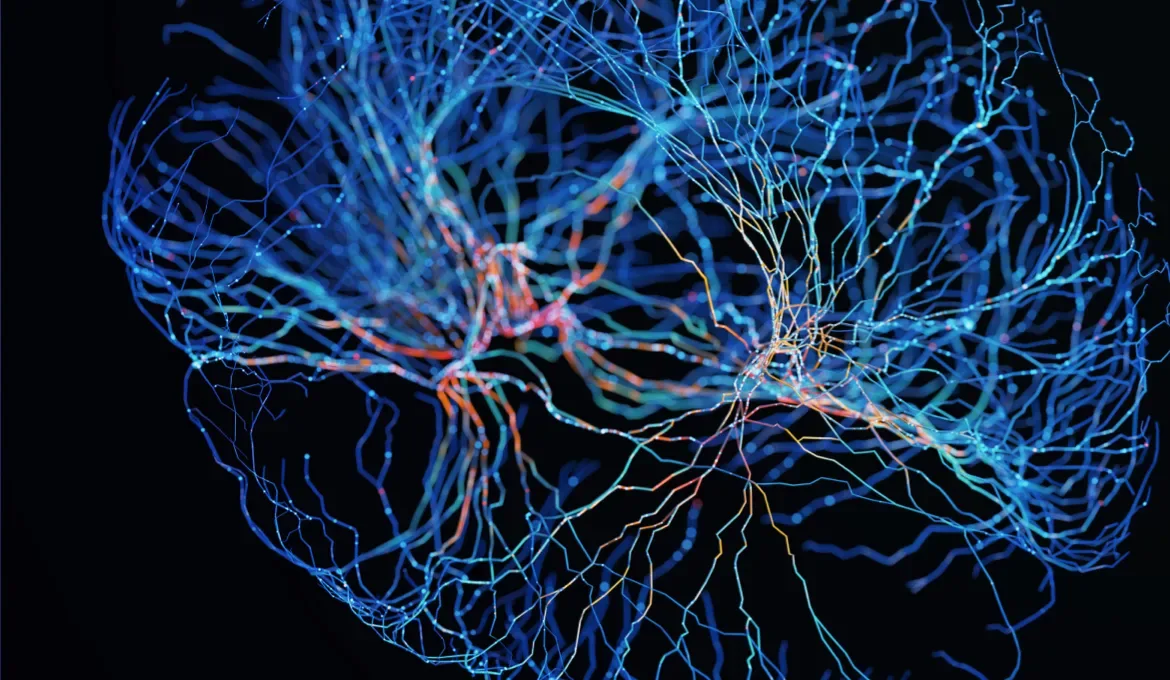
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by dysfunction of dopaminergic neurons in the substantia nigra and the accumulation of α-synuclein within dopamine-producing neurons.1
Motor features used as part of the Movement Disorder Society diagnostic criteria of PD include the presence of bradykinesia, in combination with either resting tremor, rigidity, or both.2

Around 50% of patients with PD may experience hallucinations and/or delusions over the course of their disease.9 PDP manifests primarily as hallucinations, abnormal perceptions without a physical stimulus in any sensory modality (predominantly visual), and delusions, false, fixed idiosyncratic beliefs that are maintained despite evidence to the contrary. Delusions are usually associated with a paranoid theme focused on the partner, such as infidelity or intent of harm.8
In 2007, the National Institute of Neurological Disorders and Stroke and the National Institute of Mental Health (NINDS-NIMH) recognized psychosis in PD as a clinically distinct diagnosis from other causes of psychosis, such as schizophrenia or delirium.8 The NINDS-NIMH proposed diagnostic criteria include the presence of one of the following characteristic symptoms that have been recurrent or continuous for at least one month in a patient with a primary diagnosis of PD: illusions, false sense of presence, hallucinations, and/or delusions.
Dopamine depletion in the dorsal striatum due to loss of nigrostriatal neurons results in the characteristic motor symptoms of PD. Serotonergic dysfunction, however, is thought to be the underlying cause of visual hallucinations that may be experienced in individuals with PD.1,3
Changes in the early stages of PD suggest a shift toward mesolimbic and mesocortical dysfunction.4 These include diminished expression of serotonin transporter (SERT) in the forebrain, as well as observations of increased serotonergic uptake in the thalamus and raphe nuclei.4,5 SERT expression in the caudate, while preserved in early PD, decreases as PD progresses, correlating with advancing disease stage.6
Upregulation of 5-HT2A receptors has been observed in the inferolateral temporal cortex, a critical structure in visual processing, as well as other portions of the ventral pathway, including the bilateral inferior occipital gyrus and right fusiform gyrus, in PD patients with visual hallucinations.3,7 This upregulation of 5-HT2A receptors in PD may be a compensatory mechanism.4
To report an Adverse Event or Product Complaint please call (844) 422-2342.